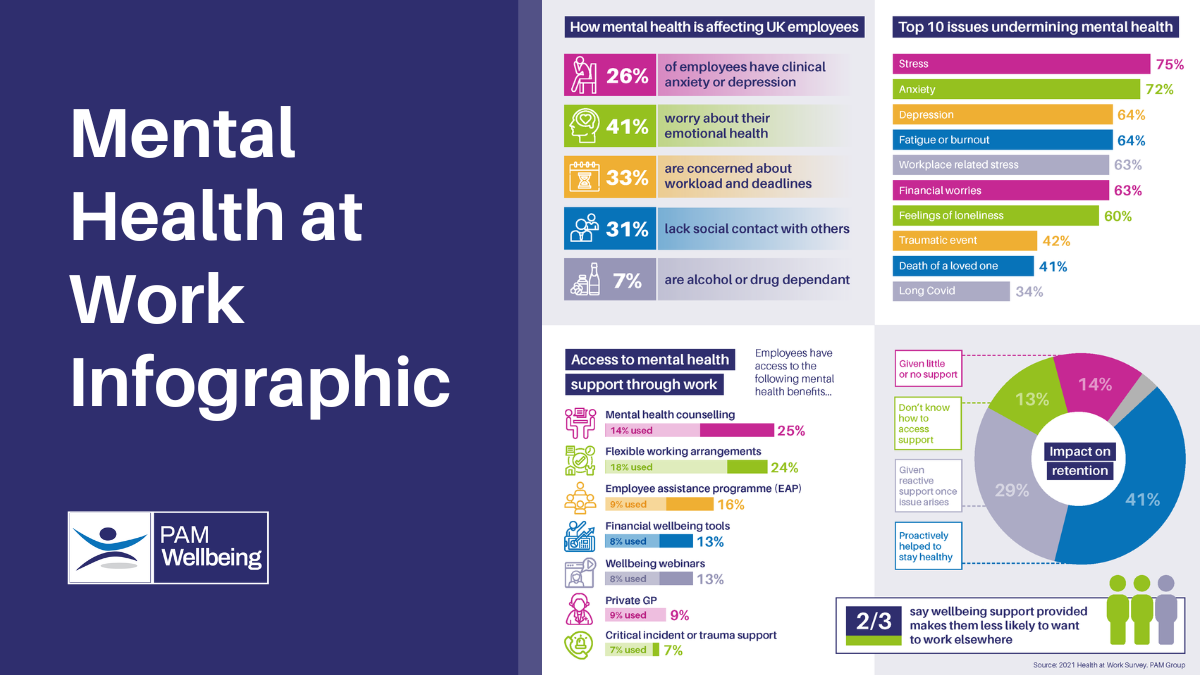
There are significant savings associated with rehabilitating the one in four employees who are clinically anxious or depressed before they go on sick leave.
Growing NHS waiting lists mean that employees referred by their GP for mental health support are typically having to wait 2-5 months to access counselling and 6-12 months to access specialist trauma therapy or cognitive behavioural therapy (CBT).
This means that by the time an employee finally gets the support they need, they will be struggling to attend or perform at work.
A far better approach is to rehabilitate them in as few as 6-12 sessions, while they’re still in work with the following proactive steps:
1. Identify those in need of support
Whether the employee is on a long waiting list to access counselling or realises all is not well with them but hopes they can recover unsupported, the chances are they will be struggling in silence for fear of recrimination, stigma or discrimination.
Essential to getting them to come forward for support is to make it clear that you understand that we all have a state of mental health that can become compromised for numerous reasons. Make it clear that you don’t want them to suffer in silence, that you have support processes in place and that they will not be penalised for utilising these as you want to help them recover.
It is also important to encourage managers to look out for people who might be struggling with their mental health and who have become noticeably distracted, error-prone, unproductive or sporadically absent. Encourage managers to talk to the individual in confidence by saying, “I’ve noticed you’re not yourself lately, is there anything going on that you need support with?” to explore the subject and see if they’re happy to be referred for support if appropriate.
2. Refer the employee for support
The type of mental health support an employee might need can differ greatly from one individual to another, and even for the same individual depending on what’s going on in their home life or at work. Healthcare practitioners use mental health assessments (such as GAD7 for anxiety or PHQ-9 for depression) to help to work out what support they might need.
Changes in mood are natural responses to some of the pressures we’re under and represent warning signs to take steps to look after ourselves. Sleep problems, panic attacks, for example, or obsessively and compulsively checking things are indicative of more serious anxiety issues. Continuous feelings of hopelessness or tearfulness may be signs of depression.
Once referred, the employee will be confidentially assessed within 1-2 weeks and a report written which will only be shared with their employer if the employee gives their consent. The aim of the report is to explain how the person is feeling, what the issues are, how their manager can support them to stay in work and what further treatment they might benefit from. Most employees are keen to share this information to help progress their recovery.
3. Invest in treatment
The treatment needed by the employee could vary from providing access to self-help education and other support services, or from debt advice to a chat with a counsellor via the Employee Assistance Programme (EAP) to more in-depth psychological services.
These in-depth psychological services might include Eye Movement Desensitisation and Reprocessing (EMDR), to help people process trauma and overcome their fear response, counselling, to talk through problems and develop coping strategies, or Cognitive Behavioural Therapy (CBT) to help them manage problems by changing the way they think or behave.
Psychological health providers, such as PAM Wellbeing, offer a Stepped-Care model, to provide the most appropriate treatment at each stage of the individual’s recovery. The intensiveness of the care may be stepped down as the individual recovers, or up if they experience a setback during their recovery.
4. Facilitate recovery
The health provider should keep the employee’s manager, and the HR contact, updated on the individual’s progress throughout their recovery and provide a report with practical and actionable recommendations on how the employer can support them to stay in work. For example, by allowing them to reduce the pressure they’re under at work for a while or start work at a later time if they have sleep issues.
If the individual was traumatised at work, due, for example, to an aggressive customer or accident, part of their therapy might involve making them feel safe in the environment where the incident happened. If they are struggling with a bereavement, complex grief or feelings of low self-esteem while they go through a divorce, they might need to work more flexibly for a time so they can attend their weekly counselling session or work from home when feeling tearful.
Throughout the individual’s recovery, every effort should be made to keep them in work, as work can be a power for good, helping the individual to have a sense of purpose and achievement. Our experience of rehabilitating employees with moderate to severe anxiety and depression also shows that quicker referrals, made while the employee is still in work, require fewer sessions and cost less than once the employee has already gone on sick leave.
5. Calculate the return on investment
Once the employee has been helped to recover, which typically takes just 6-12 weeks, while they’re helped to stay in work, it’s important to calculate the return on your investment. This will help you to justify the initiative to the board or chief financial officer so that you can help more people in future.
When calculating the business benefits, it’s important to not only consider direct costs, such as any sickness absence, but also indirect costs, such as the cost of replacement staff to cover and any contracts that might not have been fulfilled in their absence. Research by Deloitte shows employers typically save £5 for every £1 invested in mental health services.
Also try to calculate less tangible human capital savings, in terms of increased loyalty, productivity and engagement from the employee and reduced staff turnover costs. If the employee is happy to share their experience, this can also be captured in writing to create a testimonial that can be shared with other employees to encourage more people to come forward for support.
Malcolm Smith is head of wellbeing development, for PAM Wellbeing
How can PAM Wellbeing help?
To find out more about our stepped-care anxiety and depression rehabilitation services, please email Malcolm Smith so he can arrange a 1:1 Teams meeting with you.